The Medical and Health Science Centre of the University of Debrecen, which is the second largest medical school in Hungary, is carrying out a comprehensive research project aimed at recognising underlying mechanisms and developing new stem cell-based therapies for treating patients suffering from advanced peripheral arterial disease.
7000 amputations annually
Peripheral arteries are the arteries that are farthest from the heart, typically in the legs. Peripheral arterial disease is a disorder that occurs when arteries in the body’s circulatory system are obstructed, and may result in the clinical amputation of the leg. About 7000 amputations resulting from peripheral arterial disease are performed each year in Hungary. In the north Alföld (Northern Great Plains) region of Hungary, where Debrecen is situated, the occurrence of peripheral arterial disease and other cardiovascular diseases are exceptionally high.
Improving blood flow
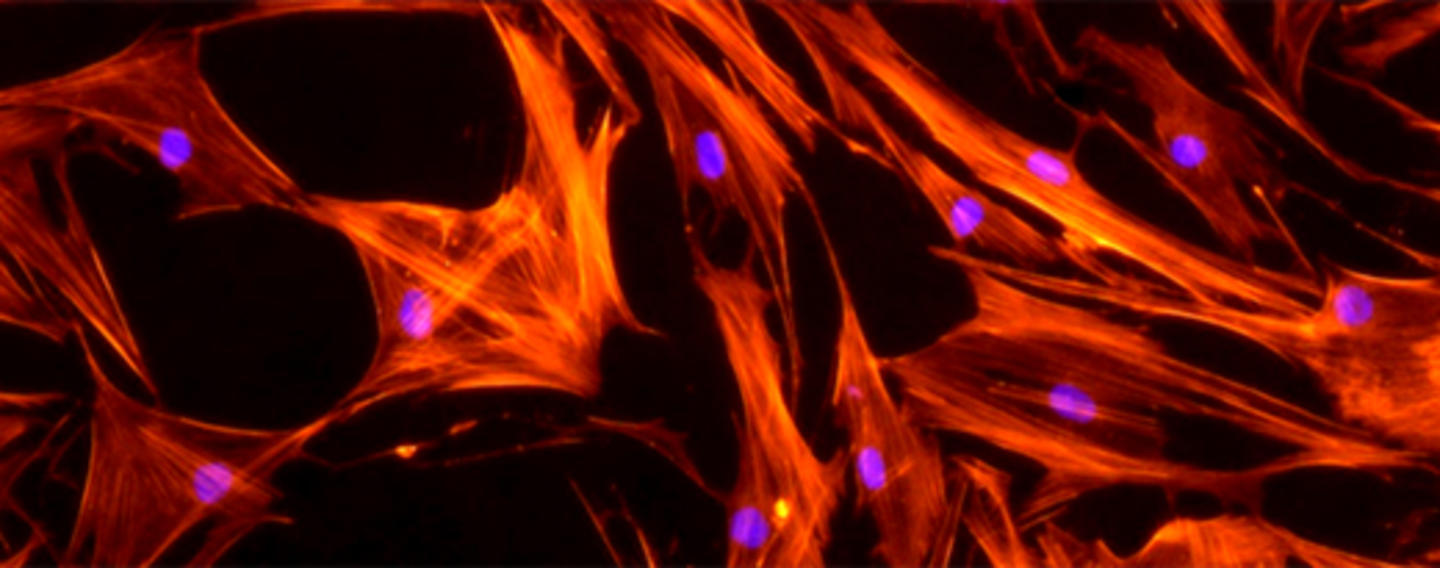
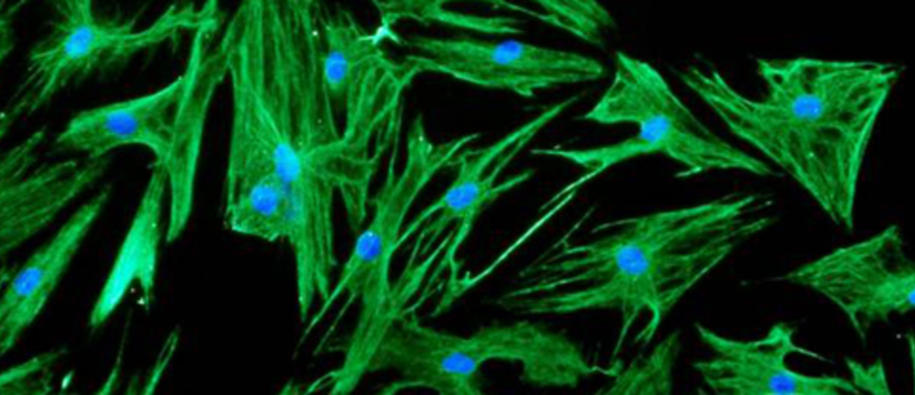
With €550 000 in support from the Norway Grants, the collaborative team of the Medical and Health Science Centre of the University of Debrecen is studying the type and characteristics as well as the mechanisms of stem- and progenitor cells with the capability to improve the blood flow in legs of patients suffering from peripheral arterial diseases. Treatment with cells that can make new blood vessels offers a unique option to prevent or postpone the need of amputation and improve the quality of life of patients. Until now, no effective medical therapies to this effect have been developed.
The Cell Therapy Group at the Stem Cell Centre at the Oslo University Hospital Rikshospitalet in Norway participates as partner in the project. More specifically, the research entails identifying the phenotype and function of tissue stem and progenitor cells involved in blood vessel formation and identification of the most suitable isolation methods. The project will not involve isolation or production of, or experimentation with human embryonic stem cells.
"Our results indicate that the bone marrow contains multiple stem- and progenitor cells with the potential to support vessel regeneration. When these cells interact with tissue- and immune cells of the inflamed milieu of the obstructed vessel, they acquire novel activities and trigger a cascade of local events that support vasculogenesis and wound healing. The complex mechanisms may involve controlled production of soluble factors, regulation of endothel cell functions, formation of new vessels, tissue regeneration, and inhibition of inflammation. These events altogether support increased blood flow, healing of ulcers and ultimately protect the leg from amputation," says Professor Dr Éva Rajnavölgyi, Head of the Immunology Department of the Medical School and Health Science Centre at the University of Debrecen.